21 October 2021
Understanding Pancreatitis - The Lesser Known Digestive System Disease
the digestive system includes many organs working in harmony to maintain health. Every organ is integral for optimal body function, but there are some organs which are less known than others. One such less known organ is the pancreas.
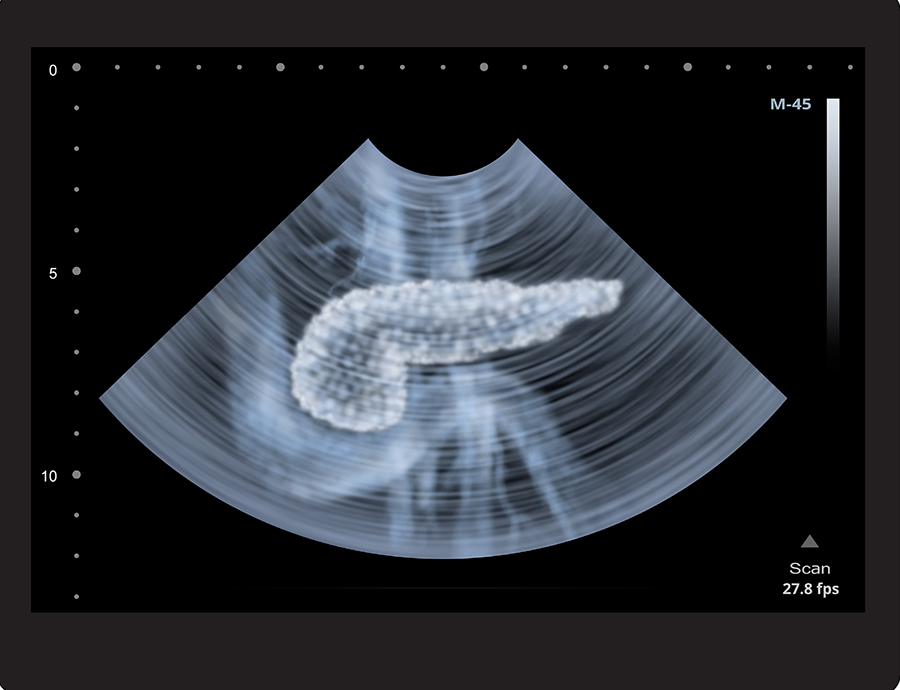
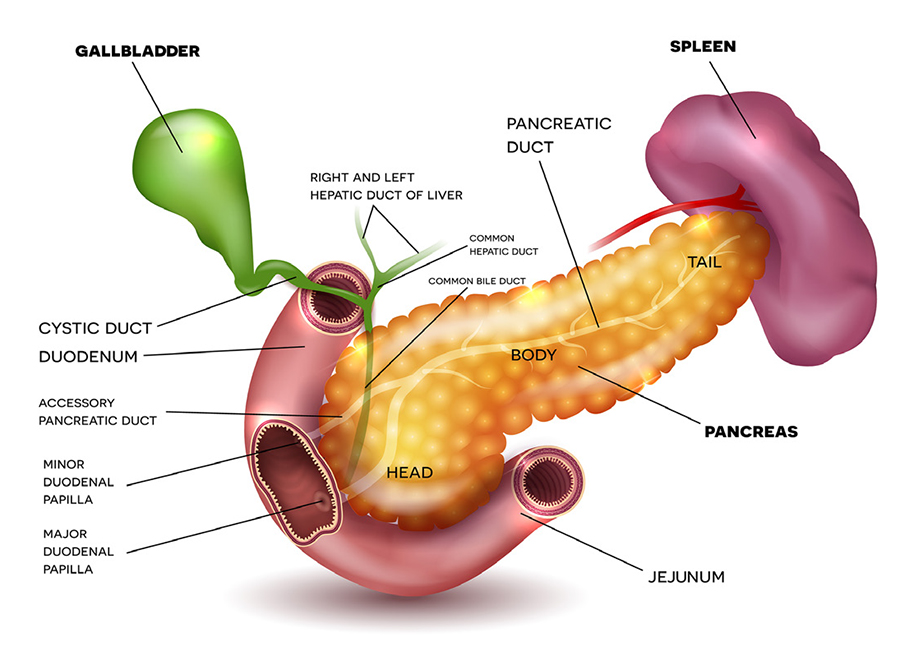
The word pancreas is derived from the Greek word pánkreas (pán = all, and kreas = flesh). The organ itself is located horizontally in the upper abdomen, deep beneath the stomach. Historically, it was believed to be a cushion for the stomach! However, it is now clear that the pancreas has two essential functions: the production of digestive enzymes and the regulation of sugar balance.
Like all body organs, the pancreas can become diseased, and one disease that can affect the pancreas is pancreatitis. Pancreatitis essentially means “swelling or inflammation of the pancreas.” Pancreatitis can be either sudden (acute) or slowly progressive (chronic). Each of these two disorders has unique features.
Acute Pancreatitis
Acute pancreatitis is a common reason for A&E department visits and hospitalisation. The swelling of the pancreas can occur due to gallbladder stones, alcohol drinking, high triglyceride, high calcium, trauma involving the abdomen (e.g. bicycle handlebar injury), certain virus infections (e.g. mumps), and endoscopic procedures related to the bile duct. Recently, COVID-19 is also implicated in causing acute pancreatitis.
In Singapore, gallbladder stones are one of the most common causes of acute pancreatitis. Patients may experience sudden severe upper abdominal pain that may also be perceived in the upper back. Typically, the pain will not be improved by over-the-counter antacids or “gastric pills”. Often, pain is associated with vomiting or fever. Confirmatory diagnosis is established by blood tests that show high levels of pancreas enzymes (e.g. amylase or lipase) in the blood. Sometimes, a doctor would recommend a computerised tomography (CT) scan or a magnetic resonance imaging (MRI) scan to establish the diagnosis. The scans are not always mandatory to confirm the diagnosis, but they are integral in the care and management of acute pancreatitis in many instances.
Treatment of Acute Pancreatitis
The treatment (of acute pancreatitis) is supportive and thankfully, most patients with mild inflammation recover well.
In general, there is no medicine to cure acute pancreatitis. The treatment is supportive and thankfully, most patients with mild inflammation recover well. However, about 10-15% of patients experience stormy disease with severe inflammation that affects multiple organs like the lungs, kidneys, etc. This group of patients is at risk of requiring intensive care, with predicted prolonged stay in hospital and real risk of death. However, with a better understanding of disease biology and natural course, improvements in critical care, advances in imaging technology and image-guided interventions, and better treatment of sepsis, clinical outcomes for patients in Singapore is on par with the highest international standards.
Once a patient recovers from the symptoms of severe acute pancreatitis, and in all patients with mild acute pancreatitis, the focus should be on treating the cause. In patients with gallbladder stones, gallbladder removal (cholecystectomy) is advocated. This surgery is common in Singapore and is routinely done as a day procedure by keyhole technique (laparoscopy). Removal of gallbladder prevents future relapses of acute pancreatitis.
In patients with alcohol abuse, complete abstinence is the key to preventing any future acute pancreatitis episode. Even a small quantity of alcohol can trigger acute pancreatitis and thus, complete abstinence is the key. It can be challenging for various reasons and specialist services are available in all acute hospitals to assist with “alcohol abuse” rehabilitation.
The doctor will actively search for a cause of acute pancreatitis to mitigate the risk of relapse. In some instances, despite detailed tests, the cause cannot be established. In such cases, removal of the gallbladder may reduce the risk of relapses. However, this must be carefully discussed with the patient.
Necrotising Pancreatitis
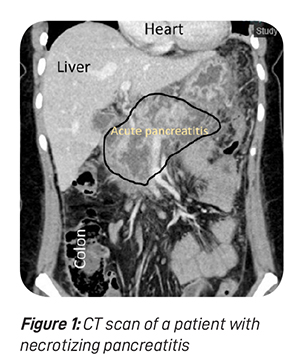
Necrosis means dead or non-viable. When a part of the pancreas or surrounding fatty tissue is dead due to severe and extensive inflammation, necrotising pancreatitis is diagnosed (see figure 1). The treatment of necrotising pancreatitis involves additional consideration for the treatment of necrotic tissue.
In olden times, urgent surgery would have been advocated. However, modern understanding dictates that doing “less is more”. If a patient’s condition is reasonably stable, any intervention is generally not advocated in order to balance between risk and gain. Interventional radiology specialists may place a “drainage tube” in and around the pancreas, if necessary, to aid in the drainage of the dirty effluent outside the body cavity. Most patients will improve with this procedure.
This procedure also allows collection of a fluid sample which can be sent for bacterial analysis to guide antibiotic treatment.
A bacterial sample can also be obtained by percutaneous (via skin puncture) or endoscopic-guided needle aspiration (via endoscopy). It is essential to administer appropriate targeted antibiotic treatment if infection is detected. Figure 2 shows a patient with necrotising pancreatitis with infection, evidenced by the gas formation in and around the pancreas. Targeted antibiotics are essential to reduce the development of resistant bacteria.
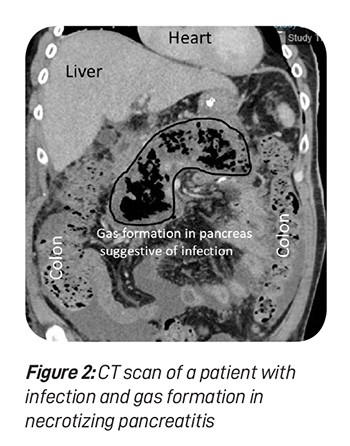
In a handful of patients where drainage does not improve the patient’s condition, surgical debridement is necessary. Historically, it was done via a big abdominal incision. Nowadays, debridement is performed by keyhole surgery, and this has revolutionised the patient recovery process. Smaller incisions reduce the risk of wound infection and surgical incision associated pain. They also facilitate shorter hospital stay and an early return to baseline body functions.
If a large portion of the pancreas is non-viable due to necrosis, the patient has a risk of enzyme deficiency (causing malabsorption) and sugar imbalance (causing diabetes). All patients with necrotising pancreatitis should be monitored for these complications, which endorses the role of multidisciplinary care.
Pseudocyst of Pancreas
In some patients, acute pancreatitis evolves into a fluid-filled cavity in the vicinity of the pancreas. This is called pseudocyst. The fluid typically contains pancreas enzymes like amylase and can sometimes be infected with bacteria. In many instances, the pseudocyst resolves naturally after a period of observation. However, pseudocyst may persist in some patients and cause symptoms like abdominal bloating, nausea, early satiety, etc. Therefore, in patients with symptoms, intervention is warranted.
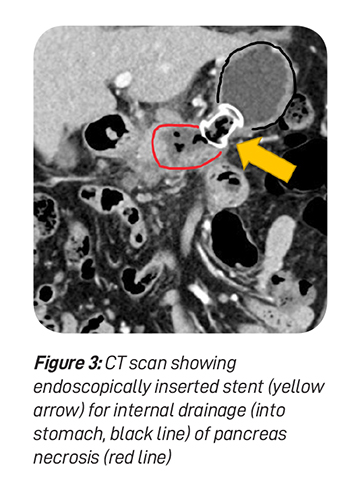
The pseudocyst requires drainage of fluid contents. The contents are typically drained internally into adjacent organs like the stomach or small intestine. The drainage procedure can be done by endoscopy (see figure 3) or surgery. Surgery can be either performed by open wound or keyholes. Pseudocysts develop more commonly following chronic pancreatitis.
Chronic Pancreatitis
Chronic pancreatitis is typically diagnosed in alcoholic patients with recurrent episodes of upper abdominal pain. It is more common in men, and has vast socioeconomic ramifications secondary to alcohol abuse and disrupted family dynamics in many patients. Chronic pancreatitis is generally confirmed on a background of a typical triad, namely, prolonged upper abdominal pain, diabetes and malabsorption. Dysregulated sugar balance mechanisms can lead to diabetes.
Reduced production of pancreas digestive enzymes leads to maldigestion of fats, increasing stool fat content. Such stool is typically bulky, has an offensive odour, floats on the toilet bowl, and is difficult to flush. In patients with these symptoms, the quality of life is affected. Patients with chronic abdominal pain may resort to regular pain killer medications, including morphine or its derivatives. Chronic medication use can transform into abuse and thus, early detection, timely counselling, and treatment are integral to care delivery.
Treatment of Chronic Pancreatitis
Treatment principles of chronic pancreatitis involve treating abdominal pain, treating the deficit of pancreas digestive enzymes with supplemental enzymes, and management of diabetes. Pancreas enzyme replacement involves swallowing enzyme-containing capsules along with meals. Typically, the enzyme is manufactured using a porcine base, which must be disclosed to Muslim patients due to religious sensitivity.

Surgery may be warranted in patients with recalcitrant abdominal pain despite optimal pain relief medication and symptomatic pseudocyst. In addition, chronic pancreatitis predisposes to pancreas cancer formation. Thus, all patients with chronic pancreatitis should be followed up for early detection of any transformation to pancreas cancer. Pancreas cancer in patients with chronic pancreatitis is generally detected due to new-onset jaundice (yellowish discolouration of skin and eyes) or growth on CT scan.
Pancreas Cancer
Pancreas cancer is an aggressive cancer with a high risk of spread to other body organs. Most patients with pancreas cancer survive less than three years despite surgical removal of cancer. In selected patients, symptoms can be managed with external radiation. In instances where the tumour causes blockage of the bile duct, the patient may develop jaundice. In such cases, an endoscopy procedure can facilitate placing a plastic or metallic tube (stent) within the bile duct to relieve jaundice. All patients with pancreas cancer should be discussed at the multidisciplinary oncology board for optimal management to provide patient-centric and evidence-based care.
Adj A/Prof Vishal G Shelat is a general surgeon with an interest in pancreas surgery. He is trained in laparoscopic and robotic pancreas surgery. Adj A/Prof Vishal is passionate about education, research, and quality improvement in clinical surgery.
He is a recipient of the National Research Foundation grant from Ministry of Health to study serum metabolomics in pancreas disorders. He is widely published and has been cited more than 3,000 times. Adj A/Prof Vishal is married with two children. In his spare time, he is a philatelist and plays chess.