
Prime Magazine October/November Issue
Strong Bones for Life
Understanding Osteoporosis and the Power of Exercise
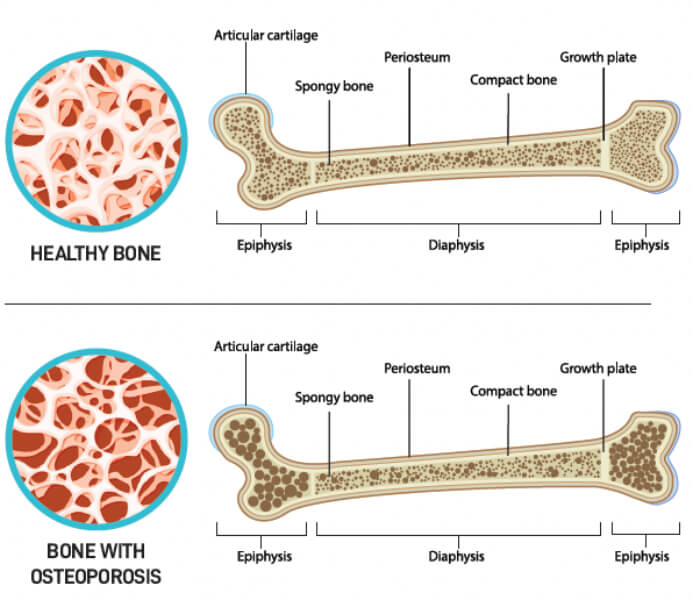
Osteoporosis is a silent threat that may reduce your quality of life and your independence as you age. It is more than just a decrease in bone density. Osteoporosis involves a complex process known as bone remodelling that is controlled by two distinct cell types: osteoclasts (“bone destroyers”), which are responsible for the periodic resorption of older bones; and osteoblasts (“bone builders”), which help to form new bone to replace bone lost. Osteoporosis happens when osteoclasts are more active than osteoblasts, resulting in net bone loss. This increases the risk of fractures, especially in the hips and spine.
In Singapore, the total number of osteoporotic fractures recorded in 2017 was 15,267. This number is estimated to increase to 24,104 in 2035, a 57.9% rise in less than 20 years (Chandran et al., 2019). Osteoporotic fractures could lead to reduced mobility and independence, affecting one’s quality of life and increasing mortality. Thus, preventing and managing this condition before a fracture occurs is crucial.
Risks and Signs of Osteoporosis
Age, gender, body mass index (BMI), physical inactivity and the use of certain steroids (e.g., for treating autoimmune conditions) are pivotal risk factors for osteoporosis. While peak bone mass typically occurs in early adulthood, the ageing process often disrupts the balance of bone remodelling, leading to gradual bone loss. Post-menopausal women may face an additional challenge, as reduction in oestrogen levels accelerates osteoclast activity and reduces osteoblast activity. Being underweight (BMI<18.5kg/ m2) is also associated with reduced bone mineral density (BMD). This may be because heavier individuals tend to achieve higher peak BMD as they exert a greater load on their weight-bearing joints.
The Osteoporosis Self-Assessment Tool for Asians (OSTA) offers a simple means of gauging one’s risk of osteoporosis (see Figure 1). However, do note that this tool only considers two risk factors: age and weight.
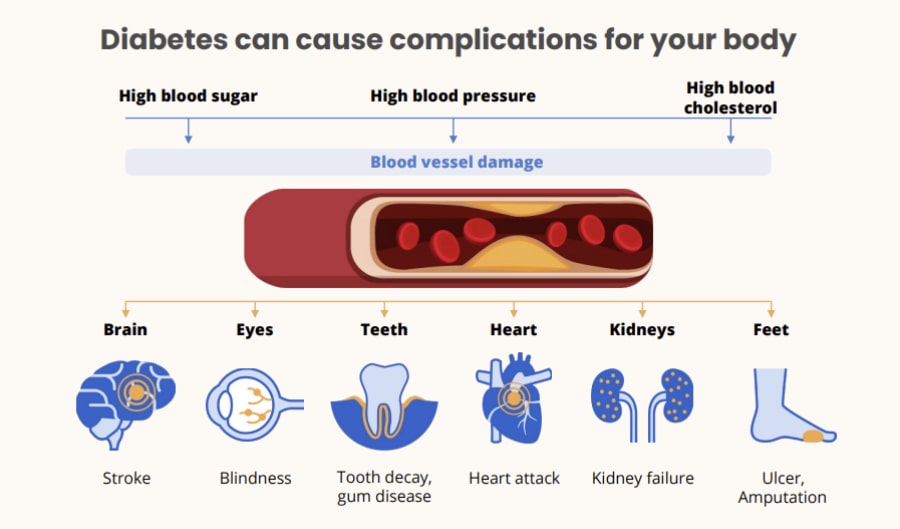 Figure 1: Osteoporosis Self-Assessment Tool for Asians (Credits: Agency for Care Effectiveness)
Figure 1: Osteoporosis Self-Assessment Tool for Asians (Credits: Agency for Care Effectiveness)
Due to its silent progression, osteoporosis often escapes notice until a symptomatic fracture occurs. However, certain later-stage indicators may point to osteoporosis, including unexplained lower back pain and a gradual loss of height over time (more than 2cm over three years) accompanied by a stooped posture. The diagnosis of osteoporosis usually involves a dual-energy x-ray absorptiometry (DXA) scan, which assesses an individual’s BMD.
Exercise as Your Ally
Exercise is an effective adjunct treatment to combat osteoporosis and slow down the progress of bone loss.
From racquet sports to dancing and running, weight-bearing exercises can stimulate osteoblast activity, fostering bone growth and preservation. Resistance exercises also protect bone health by increasing mechanical stress on the bone through muscle activation. Exercises that challenge one’s balance and improve back extensor strength can increase postural stability, and help to prevent fall-related fractures. In contrast, avoidance of physical activity and a sedentary lifestyle are thought to unload the skeletal system, resulting in weaker bones and a greater risk of fractures.
If you have concerns about starting or are unsure about the right exercises for you, do seek advice from a physiotherapist, who can prescribe an exercise programme tailored to your needs while ensuring your safety during exercise.
Strong, Steady and Straight
,p>The British Medical Journal (BMJ) recommended a useful three-pronged approach to exercise for osteoporosis in 2022 (see Figure 2). The three prongs are:
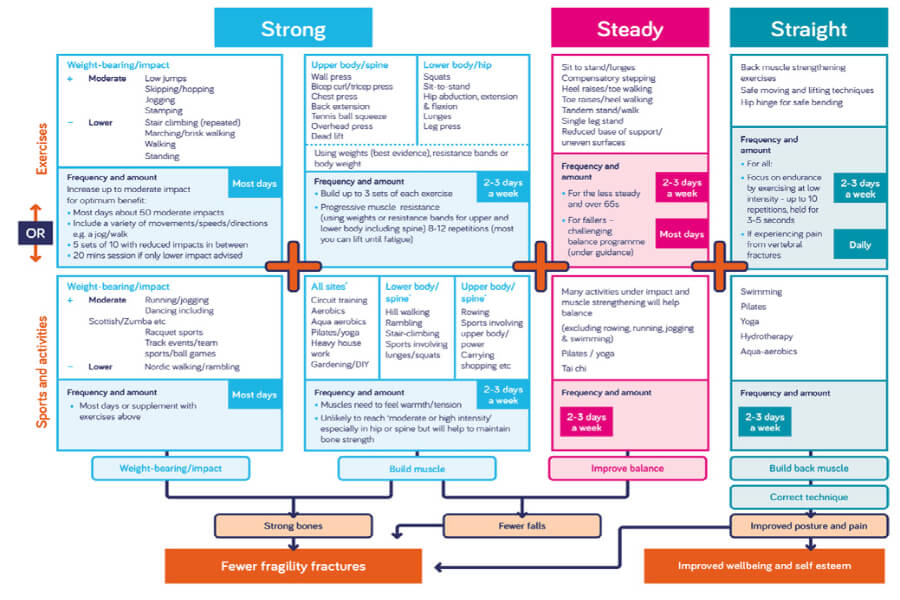 Figure 2: Strong, Steady and Straight Framework (Brooke-Wavell et al., 2022)
Figure 2: Strong, Steady and Straight Framework (Brooke-Wavell et al., 2022)
STRONG: Focus on exercises that help to promote muscle and bone strength, and prevent fractures. These include weightbearing or impact exercises such as jogging and hopping, and resistance exercises for building muscles. It is recommended to perform impact exercises on most days of the week, and resistance exercises 2-3 times a week for three sets of 8-12 repetitions. Target skeletal sites could be considered when choosing resistance exercise types. For instance, exercises such as squats, lunges and wall push-ups can be used to load the spine, femur (thigh bone) and forearm. Intensity can be modified with exercise bands or weights.
 Squats and wall push-ups (Credits: Tan Tock Seng Hospital Physiotherapy Department)
Squats and wall push-ups (Credits: Tan Tock Seng Hospital Physiotherapy Department)

STEADY: Prioritise balanceimproving exercises like dance and tai chi to improve balance, reduce the risk of fall-related fractures, and maintain independence.
Other ways to challenge our balance systems include exercises performed with a reduced base of support or on uneven surfaces, such as heel raises, tandem standing or foam cushion standing.
However, supervision is advised when performing balance exercises, especially for individuals with a history of falls. It is recommended that balance exercises be performed at least 2-3 times a week.
STRAIGHT: Engage in exercises that improve posture, such as swimming. These exercises target back extensor strength, which may counteract the progressive muscle weakness and spinal deformities observed in osteoporotic individuals, and improve standing balance.
It is recommended to perform these exercises 2-3 times a week.
 Pectoralis stretch (Credits: Tan Tock Seng Hospital Physiotherapy Department)
Pectoralis stretch (Credits: Tan Tock Seng Hospital Physiotherapy Department)
Safety in Exercise
For sedentary individuals new to an exercise routine, you may want to start at a lower, comfortable intensity, focusing on correct technique and posture. For those without osteoporosis, daily physical activity and exercise are advised to keep osteoporosis at bay.
While those with osteoporosis may fear that exercise might increase the risk of intra-session fractures, in fact, most observational studies show that exercise regimes, when performed appropriately, do not increase the risk of adverse events like fractures.
For osteoporotic individuals without fractures, certain manoeuvres such as end-range, sustained loaded flexion exercises (e.g., sit-ups, certain yoga positions with extreme spinal bending, etc.) should be modified or avoided to ensure safety. Safe lifting techniques, including keeping your upper back straight, hip hinging and engaging your abdominal muscles during lifts, are also recommended. For osteoporotic individuals with fractures, it is best to seek individualised advice from a registered physiotherapist to maximise effectiveness and ensure safety during the start of a new exercise programme.
CONCLUSION
With appropriate precautions, exercise is safe and beneficial for individuals with osteoporosis; it helps to prevent the onset of osteoporosis. While it may seem daunting to start exercising regularly, it is really not as difficult as it looks. Start by including small bouts of physical activity or exercise in your daily lives, such as doing sit-to-stands while watching the television, taking the stairs instead of the lift, or even dropping off one bus stop before your destination. There is no better time than now to take proactive steps toward stronger, healthier bones.
Ms Tay Ming Yi is a registered physiotherapist working at Tan
Tock Seng Hospital, with experience caring for individuals with
diverse medical histories, including chronic illnesses, brain
injuries and musculoskeletal disorders. Through her practice,
she hopes to inspire patients to view physical activity and
exercise as necessary, enjoyable and engaging.
Tan Tock Seng Hospital