Download English PDF, 916KB, PDF
Download Chinese PDF, 740KB, PDF
What is Joint Hypermobility Syndrome?
Hypermobility is used to describe your joints that are unusually flexible, resulting in larger range of movement. When multiple joints are affected and associated with pain without any underlying disease, you may be having joint hypermobility syndrome (JHS).
JHS is different from other disorders that cause local joint hypermobility and joint looseness, such as Ehlers-Danlos syndrome and Marfan syndrome. These heritable disorders are very rare but may have serious complications.
Left (top and bottom): Thin, stretchy skin and hypermobile joints due to Ehlers-Danlos syndrome;
Right: Hypermobile long fingers in a patient with Marfan’s syndrome able to wrap around opposite wrist.
Photos retrived from British Medical Journal.
What Causes Hypermobility?
Hypermobility unassociated with other underlying disease occurs in 4 to 13% of the general population. It is commonly seen in healthy people who do not have any complaints about it. Causes include:
- Younger age. As you get older, tendency of getting hypermobility generally decreases
- Female gender
- Genetics (e.g. people of African, Asian and Middle Eastern descent)
- Difficulty in swallowing (may result in choking or accidental inhalation of food into the lungs when eating)
- Coughing and shortness of breath due to lung inflammation
- General symptoms like lethargy, fatigue, weight loss and poor appetite.
Due to excessive joint looseness, hypermobility may lead to wear and tear of joint surfaces, and strains on soft tissue structures around the joints. These result in joint pain and JHS. Some people with hypermobility may have affected sense of joint movement, causing an inability to sense that joints are overstretched or injured.
What are the Symptoms and Signs of JHS?
People with JHS may experience the following:
- Joint stiffness and pain (usually in the later part of the day)
- Muscle strain or pain
- Frequent joint sprains, strains and dislocation
- Difficulty in swallowing (may result in choking or accidental inhalation of food into the lungs when eating)
- Ability to contort body parts into strange shapes (“double-jointed”)
Associated signs include:
- Thin skin
- Scoliosis, pes planus (“flat feet”)
- Hernias and varicose veins

Left: Flexible index finger “(double-jointed”); Right: “Flat foot”.
How is JHS Diagnosed?
Diagnosis of JHS is one of exclusion, particularly in those with painful and swollen joints. A detailed history is taken and physical examination performed to exclude inflammatory, infective and autoimmune causes.
To determine hypermobility, the following questions may be asked:
- Have you ever been able to place your palms flat on the floor without bending your knees?
- Have you ever been able to bend your thumb to touch your forearm?
- As a child, were you able to contort your body into strange shapes or do splits?
- As a child or teenager, have you ever dislocated your shoulder or knee cap on more than one occasion?
- Radiological Imaging – Imaging may be performed to determine the diagnosis (e.g. MRI to identify abnormal muscles) and evaluate extent of disease (e.g. chest X-ray and high resolution CT scan to detect lung involvement).
- Do you consider yourself “double-jointed”?
Beighton score will be calculated by doing five simple manoeuvres to measure generalised joint looseness, which is indicated by a score of four or more out of nine.
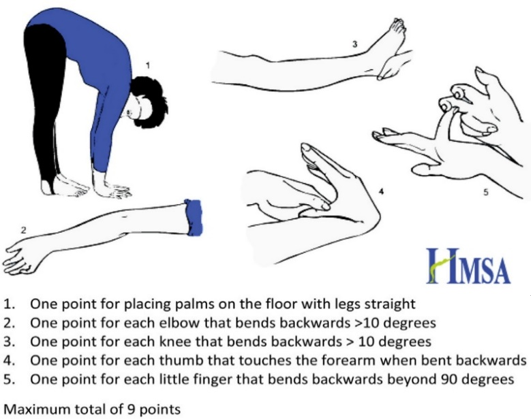
Beighton’s score.
Photo retrieved from Hypermobility Syndromes Association.
Further investigations are generally not required, unless the symptoms and signs are suspected to have other causes, such as infection or autoimmune disease.
What is the Treatment for JHS?
For management of acute symptoms:
- Rest and abstain from activities that may further strain your affected joints
- Physical therapy and joint protection (e.g. splints, taping and applying elastic bandages)
- Non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol can be used for pain control
The long-term management for JHS is achieved through changes in lifestyle and exercise regimen, joint protection, and observing proper body mechanics.
Strategies include:
- Strengthening programmes and focused exercises to improve muscle strength, balance and coordination. These will in turn improve joint stability and sense of joint movement
- Stretching techniques targeted at tight muscles without over-stressing the joints
- Using supportive splints and appropriate footwear
- Taking painkillers before more strenuous physical activities
What is the Outlook for JHS?
Most people with regular joint hypermobility do not show symptoms of JHS and live their lives without any joint ailments. If you suffer from JHS, the outlook is excellent with just a simple adjustment of your way of life to reduce the frequency of joint symptoms. Proper care of your joints early in life will reduce the chances of you developing degenerative joint disease (secondary osteoarthritis) in the future.