Adequate nutrition is essential for good bone health. Nutrition supports the continuous formation of new bones to replace the continuous loss of old bones throughout life. The body’s bone mineral density (BMD) peaks at around 20 years of age, when the bone is replaced much more quickly than it is lost. After which, bone formation replaces just about as much bone is lost; with age, bone loss outpaces bone formation.
Prolonged net bone loss can cause osteoporosis, a bone disease characterised by low bone mass, decreased bone strength and increased risk of fractures. A recent local study found that 1 in 2 elderly aged 60 and above are at risk of osteoporosis, with a higher risk found among females aged between 75-85 years of age.
Additionally, over the past 3 decades, cases of hip fractures have increased 5 times in post-menopausal women aged 50 years and above. In men of the same age group, the increase is 1.5 times. According to experts, hip fractures can lead to prolonged hospitalisation. They also affect mobility and may even cause disability. Suffering an osteoporotic fracture can be life-changing as it can affect one’s quality of life - by impairing the person’s ability to perform daily activities. Therefore, it is of vital importance to have adequate nutrition to support and build strong bones.
Calcium and Vitamin D
The body uses calcium to build strong, healthy bones and teeth, while vitamin D is needed to absorb calcium. Thus, adequate calcium and vitamin D intake is integral to optimal bone health; this is even after peak bone mass is attained. As calcium is not made in the body, it must be acquired through our food intake. Calcium-rich foods include dairy products and fish with edible bones. For individuals on a vegan diet or who are lactose-intolerant, calcium-fortified foods and nondairy sources are important alternatives. Use Table 1 to help you achieve the daily recommended calcium intake of 800mg (for adults aged 19-50 years) and 1000mg (for adults aged 51 years and above) respectively. On the other hand, vitamin D can be obtained through adequate sun exposure (5-30 minutes of sunshine between 10am and 3pm) or from food sources detailed in Table 1.
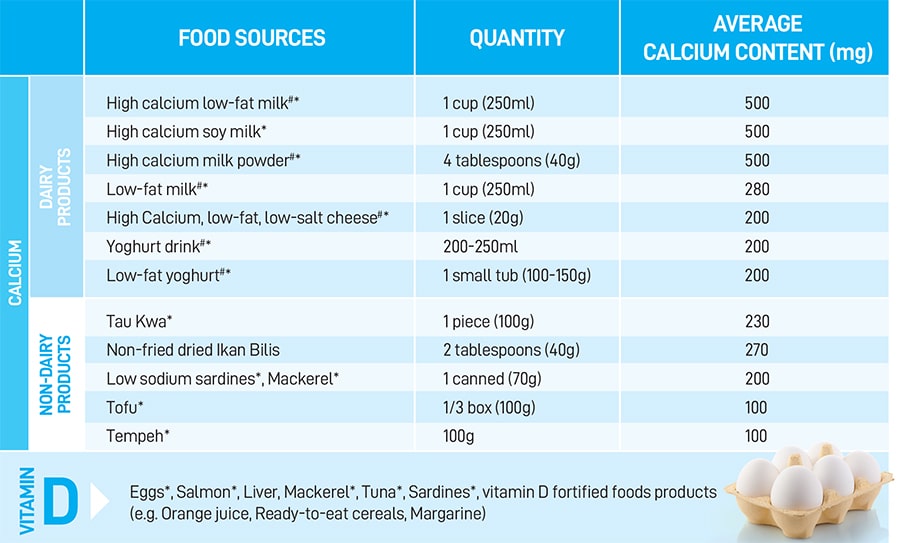 Table 1: Food sources of key nutrients for bone health (Information sources: Health Promotion Board and product packaging)
Note: # Contains lactose * Good protein sources
Table 1: Food sources of key nutrients for bone health (Information sources: Health Promotion Board and product packaging)
Note: # Contains lactose * Good protein sources
Calcium and Vitamin D supplements
Research examining the impact of taking in calcium from diet versus supplements on bone health has produced mixed results. Excessive calcium supplementation may increase the risk of heart attack, whereas increased calcium intake from diet does not. However, calcium supplements may be advised for individuals with medical conditions (inflammatory bowel disease or celiac disease) or those on medications (long-term steroids) known to decrease calcium absorption. While evidence shows no clinically significant benefit from vitamin D supplementation on bone health, vitamin D supplementation does improve serum vitamin D levels among those who may be at higher risk of deficiency, including frail elderly with minimal sunlight exposure, and individuals who are veiled or who has dark skin.
Other important nutritional considerations
Besides calcium and vitamin D, there are other important nutritional considerations for optimal bone health: Adequate protein intake (including meat, fish, egg, tofu, tau kwa and dairy products): Sufficient protein intake is integral to maintaining bone structure and growth. According to information from the Health Promotion Board, you should aim for 2-3 servings of protein every day.
Phosphorous: Phosphorous, along with calcium, is needed for the maintenance of good bone health. As phosphorous is naturally found in protein-rich foods, adequate protein intake will usually result in sufficient phosphorous intake.
Reduce sodium consumption: High sodium intake increases calcium loss, which is associated with lower BMD. You can aim to reduce sodium intake by limiting the consumption of outside food, soups, sauces, canned foods and processed foods, including cured meats, preserved meats and preserved vegetables. As much as possible, choose fresh ingredients, and use low or no-sodium added food products.
Reduce caffeine intake: Caffeinated beverages, such as coffee and tea, may cause bone loss by decreasing calcium absorption. Caffeinated sodas (e.g. cola drinks) contain both caffeine and phosphoric acid, which draws calcium from bones. Limit the consumption of these beverages to 3 or less cups per day. Decrease alcohol consumption: Alcohol consumption draws
calcium from the bone. Thus, chronic heavy drinking increases the risk of osteoporosis. As much as possible, alcohol should be avoided or limited to 2 standard drinks per day (for males) and 1 standard drink per day (for females). A standard drink is either 330ml regular beer, 100ml wine or 30ml hard liquor. There should also be at least 2 alcohol-free days per week.
Conclusion
In conclusion, adequate calcium, vitamin D and protein intake through a balanced, varied diet is recommended. For individuals who are unable to optimally obtain calcium and vitamin D from food sources and sunlight, appropriate supplementation of these important nutrients may be considered. Limiting sodium, alcohol and caffeine intake can also support good bone health.