Patients undergoing partial or total knee replacement surgery look forward to resuming or even improving their daily lives, and long hospital stays run counter to that. In 2017, a multidisciplinary team of therapists, surgeons, nurses, and care coordinators came together with a clear, collective vision: to help patients go home earlier after knee surgery.
To understand the challenges in discharging patients home sooner, the team conducted an in-depth study of existing workflows, which revealed opportunities for better coordination of care and earlier post-surgery mobilisation.
Beginning with the destination in mind
Together, they transformed the entire care process to bring discharge planning to the beginning of the patient's care journey. Specially trained care coordinators now engage patients and families once surgery has been scheduled, including rehabilitation guidance and safety education.
Lim Zhi Hui, an Advanced Scope Care Coordinator with the orthopaedic team, described the process: "We handle a large part of pre- and post-surgery counselling, like education on post-surgery needs so that patients and families can arrange for care and home safety ahead of time. We also schedule home-based nursing and therapy care within patients' homes, and check back in with patients regularly to ensure they are recovering well even after they leave the hospital."
Technology is also part of the recovery journey. On top of teleconsultations for counselling and wound care, the team is
trialling a mobile app that guides patients from pre- to post-op care. The app aims to reinforce exercises, enhance pain management, and provide real-time feedback to the care team right from patients' homes and the community.
Walking the journey one step at a time

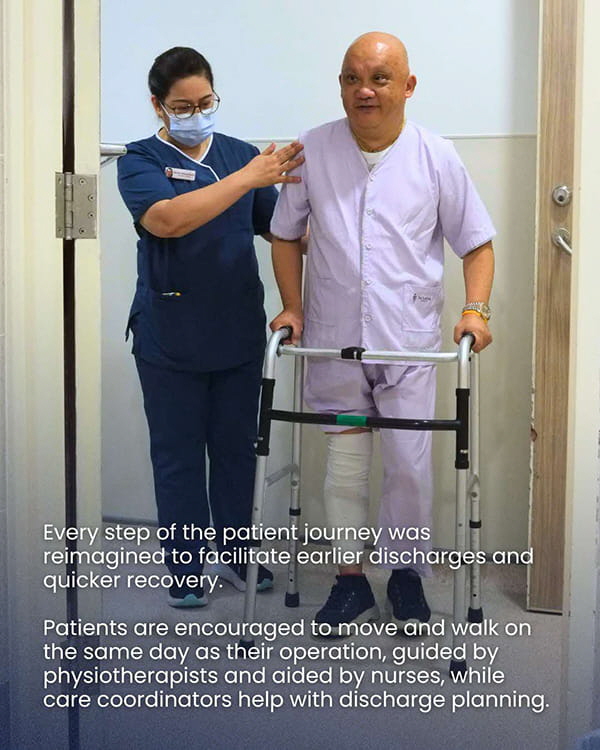
Early mobilisation is a key part of patients' recovery process; across the world, evidence has proven that getting patients to move and walk as soon as a few hours after surgery makes a big difference to their recovery.
"We tightened manpower coordination to ensure that physiotherapists are able to review patients' conditions and needs on the operation day itself whenever possible," said Principal Physiotherapist Clara Wong.
Day surgery ward nurses are also trained to mobilise patients after physiotherapists' review and outside of therapy sessions, increasing the amount of time patients spend moving and getting stronger.
Achieving safe, quicker recovery through innovative teamwork
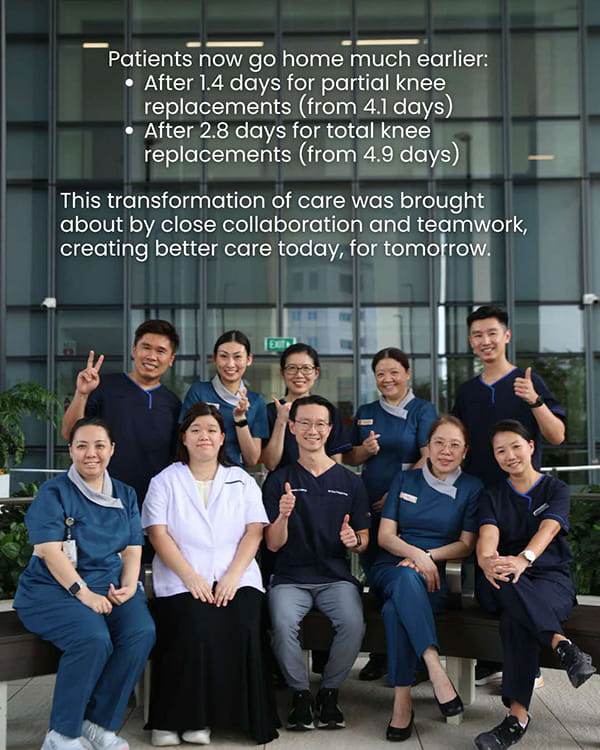
After many iterations and constant improvement of processes, average stays fell from 4.1 to 1.4 days for partial knee replacements, and from 4.9 to 2.8 days for total knee replacements. These numbers have been sustained over five years, with no increase in complication rates.
In recognition of their efforts in transforming care and recovery, the team was awarded the Healthcare Humanity Award for Collaboration in 2025 - an honour bestowed upon healthcare professionals and staff who have demonstrated exemplary care, compassion, and humanity in their work.
Together, they have given patients a faster return to daily life, highlighting the care that we deliver today, for tomorrow.