What is a Permanent Pacemaker (PPM)?
A pacemaker is a small electronic device implanted in the chest, just beneath the skin below the collar bone. It functions to reduce the symptoms caused by abnormally slow heart rhythm. The pacemaker is capable of monitoring the heart rhythm. When the heart is beating normally, the device remains inactive. If the heart beats too slowly, the pacemaker delivers a small electrical current to the heart to stimulate the heart to beat at a normal rate. Modern pacemakers are unobtrusive and do not affect daily activities.
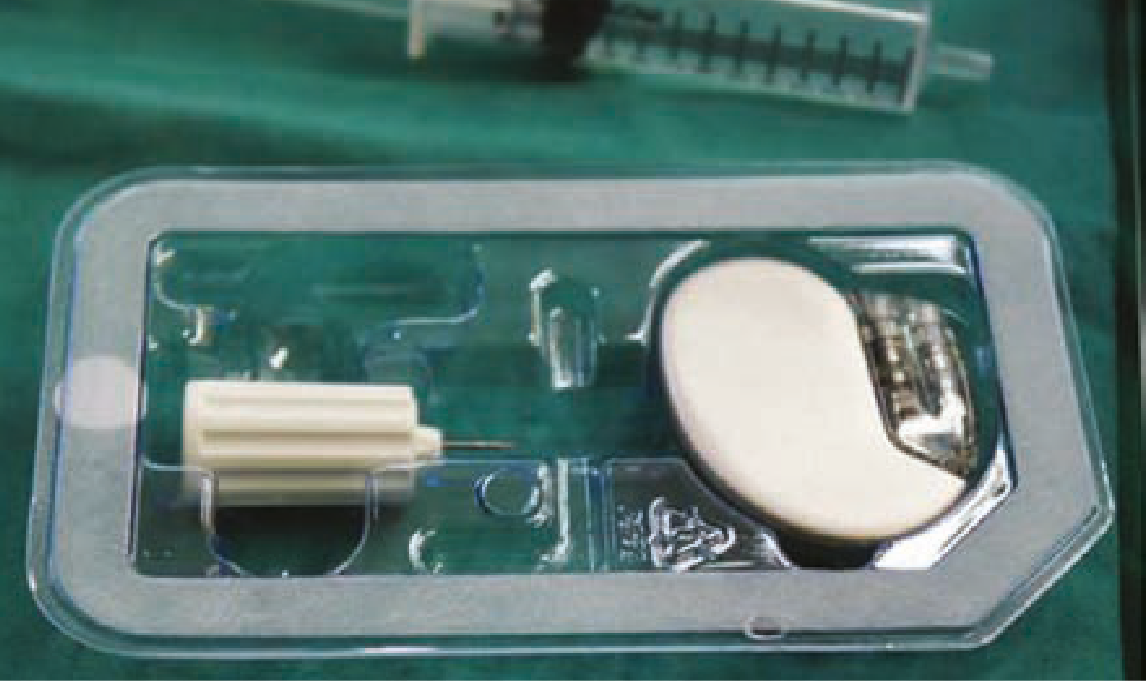
Example of a pacemaker
A pacemaker system consists of 2 parts: the pulse generator and wires with sensors (called electrodes) on one end.
The pulse generator houses the battery and tiny computer. The battery usually lasts about 7 to 10 years, after which the entire pulse generator needs to be changed.
The electrodes detect and monitor the heart rhythm. It transmits energy from the pulse generator to pace the heart if required. The wires are inserted into the heart via the veins from the upper chest.
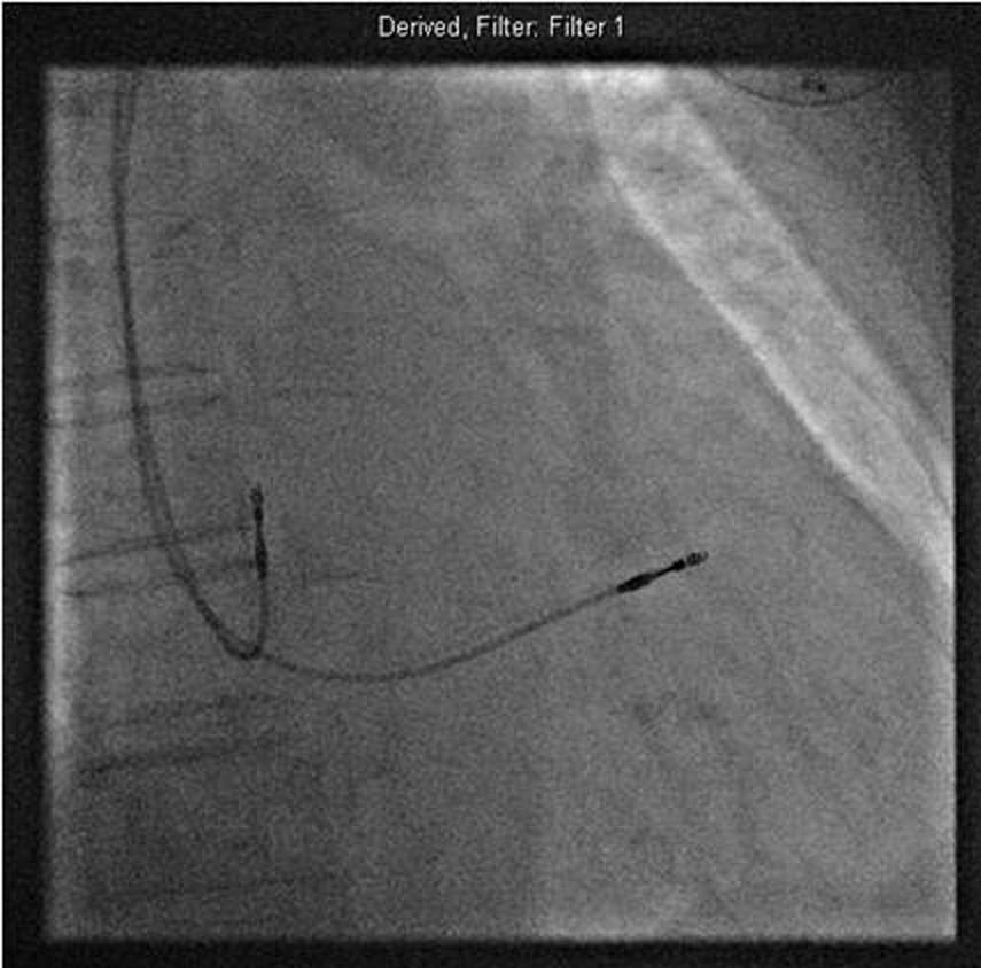
X-ray guided implantation ofthe pacemaker leads
Why Do I Need a PPM Implantation?
Unusually slow, fast or irregular heart rhythms can severely affect the heart's ability to pump blood throughout the body. This may cause symptoms such as:
When these rhythm abnormalities cannot be corrected by medications, become intolerable or pose a danger to your life, your doctor may recommend a PPM to be implanted.
What Happens During PPM Implantation?
Before the Procedure
Some routine blood tests and electrocardiograms (ECG) will be performed. The procedure usually lasts about one hour and is performed in the Invasive Cardiac Laboratory. You will need to be warded for 1 to 2 days for the implantation. You will need to sign a consent form after you have been given details of the procedure and its risks, benefits and alternatives.
If necessary, hair on your chest will be shaved, and cleansed with a special soap to keep the area of insertion sterile to prevent infection. Sterile drapes will then be used to cover you from your neck to feet. A soft strap will be placed across your waist and arms to prevent your hands from coming into contact with the sterile field.
A small plastic tube or cannula will be inserted into one of the veins on your hand to facilitate the injection of medications. Just before the procedure, you will be given an antibiotic injection to prevent wound infection and medication through the cannula to make you drowsy. However, do note that you may not be fully asleep.
During the Procedure
After the injection of anaesthetics, a small cut is made in the upper chest to create a small "pocket" under the skin to accommodate
the pulse generator. One end of the pacemaker wire is connected to the pulse generator while the electrode end of the wire is inserted through a vein in the upper chest and is positioned in the heart with the X-ray guidance.
After the Procedure
Upon returning to the ward, you will be required to lie flat in bed until the next day. Your arm on the side of the implantation may be held in a sling to avoid any big movements.
You will be given regular antibiotic injections for a day followed by oral antibiotics for about 5 days. A chest X-ray will be performed the day after the procedure to check the position of the PPM and identify potential complications. The PPM will also be programmed and checked by a technologist. Most patients can be discharged 1 to 2 days after the implantation.
Upon discharge, you will be given an appointment for a follow-up at the Pacemaker clinic in a week's time. The waterproof dressing should not be removed until you return for your review. The stitches need not be removed as they are absorbable. After your first review, your doctor will arrange for regular check-ups to ensure that the PPM is functioning normally and to electronically program the PPM to suit your heart's requirements.
Preparing for the Implantation of a PPM
You will need to fast for at least 6 hours before the implantation.
What Precautions Do I Need to Take After the Procedure?
1. Inform your doctor immediately if you have these symptoms:
2. Avoid any big movement of the arm on the affected side such as lifting the arm above your head and lifting a load of more than 5kg during the first week after implantation.
3. Complete the course of antibiotic medication prescribed upon discharge.
4. Remember to inform all your attending doctors that you have a PPM implanted.
5. Return for regular check-up at the appointed dates so that you derive the greatest benefits from the PPM.
6. Carry the temporary identification card which you will receive after the implantation. It indicates what type of PPM and electrodes you have, the date of implant and the doctor who performed the implant, in the case that medical care is needed. Within three months, you will receive a permanent card from the PPM company.
7. If you feel unwell after the PPM implantation, please contact the Centralised Appointment Line (6357 7000) to make an earlier appointment with the Pacemaker Clinic.
If you have any queries regarding these instructions, please contact your doctor.
What are the Potential Risks?
The procedure is extremely safe, with a low risk of complications. However, some potential risks include:
Minor side effects, such as pain, bleeding and bruising at the implant site, which can be easily treated.
Pneumothorax, a rare complication whereby the lining of the lung is accidentally punctured during the insertion of the pacemaker wire. Air then leaks into the chest cavity, causing the lung to collapse. This condition can be treated with the insertion of a chest tube to allow air to escape and the lung to re-expand.
Infection of the implant site, a rare but serious side effect requiring antibiotic therapy and/or surgical removal of the entire PPM system if the condition is severe.
When Will the Pacemaker Be Removed?
The pacemaker and wires will not be removed once implanted except in the following situations:
Upon death of the patient, the pulse generator has to be removed from the body before cremation.
The pulse generator will be removed and replaced when it is near the end of its battery life.
The pulse generator and the wires may have to be removed if infection occurs at the site of implant.